Background: Fetal macrosomia, defined as a birth weight ≥4,000 g, may affect 12% of newborns of normal women and 15-45% of newborns of women with gestational diabetes mellitus (GDM). The increased risk of macrosomia in GDM is mainly due to the increased insulin resistance of the mother. In GDM, a higher amount of blood glucose passes through the placenta into the fetal circulation. As a result, extra glucose in the fetus is stored as body fat causing macrosomia, which is also called ‘large for gestational age'. This paper reviews studies that explored the impact of GDM and fetal macrosomia as well as macrosomia-related complications on birth outcomes and offers an evaluation of maternal and fetal health. Summary: Fetal macrosomia is a common adverse infant outcome of GDM if unrecognized and untreated in time. For the infant, macrosomia increases the risk of shoulder dystocia, clavicle fractures and brachial plexus injury and increases the rate of admissions to the neonatal intensive care unit. For the mother, the risks associated with macrosomia are cesarean delivery, postpartum hemorrhage and vaginal lacerations. Infants of women with GDM are at an increased risk of becoming overweight or obese at a young age (during adolescence) and are more likely to develop type II diabetes later in life. Besides, the findings of several studies that epigenetic alterations of different genes of the fetus of a GDM mother in utero could result in the transgenerational transmission of GDM and type II diabetes are of concern. Show
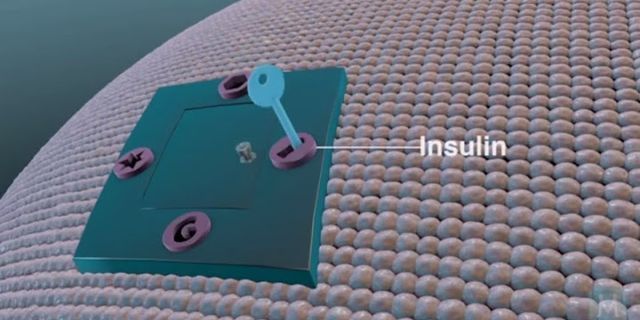
© 2015 S. Karger AG, Basel Key Messages• Fetal macrosomia, resulting from fetal hyperinsulinemia in response to maternal diabetes, might be a predictor of later glucose intolerance. • Maternal diabetes during pregnancy can lead to a transgenerational transmission of diabetes risk. • Fetuses of obese women with gestational diabetes mellitus have a higher risk of developing macrosomia than those of nonobese women with gestational diabetes mellitus. IntroductionGestational diabetes mellitus (GDM) is defined as glucose intolerance of variable degrees with an onset, or first recognized, during pregnancy. About 15-45% of babies born to diabetic mothers can have macrosomia, which is a 3-fold higher rate when compared to normoglycemic controls. Macrosomia is typically defined as a birth weight above the 90th percentile for gestational age or >4,000 g. Unlike maternal hyperglycemia, maternal obesity has a strong and independent effect on fetal macrosomia [1]. Gestational age at delivery, maternal pre-pregnancy body mass index (BMI), pregnancy weight gain, maternal height, hypertension and cigarette smoking also have a significant impact. When obese women were compared to normal-weight women, the newborns of obese women had more than double the risk of macrosomia compared to those of women with normal weight [2]. Data from the Diabetes in Early Pregnancy Study indicate that fetal birth weight correlates best with second- and third-trimester postprandial blood sugar levels and not with fasting or mean glucose levels [3]. When postprandial glucose values average 120 mg/dl or less, approximately 20% of infants can be expected to be macrosomic, and if the glucose values are as high as 160 mg/dl, the rate of macrosomia can reach up to 35%. Macrosomic fetuses in diabetic pregnancies develop a unique pattern of overgrowth, involving the central deposition of subcutaneous fat in the abdominal and interscapular areas [4]. They have larger shoulder and extremity circumferences, a decreased head-to-shoulder ratio, significantly higher body fat and thicker upper-extremity skinfolds. Because fetal head size is not increased, but shoulder and abdominal girth can be markedly augmented, the risk of Erb's palsy, shoulder dystocia and brachial plexus trauma is more common. However, skeletal growth is largely unaffected. Data from the Australian Carbohydrate Intolerance Study in Pregnant Women (ACHOIS) demonstrated a positive relationship between the severity of maternal fasting hyperglycemia and the risk of shoulder dystocia, with a 1-mmol increase in fasting glucose leading to a 2.09 relative risk for shoulder dystocia [5]. Macrosomia is associated with excessive rates of neonatal morbidity. Macrosomic neonates have 5-fold higher rates of severe hypoglycemia and a doubled increase in neonatal jaundice in comparison with the infants of mothers without diabetes [6]. In addition, there appears to be a role for excessive fetal insulin levels in causing accelerated fetal growth. In a study which compared umbilical cord sera in infants of diabetic mothers and controls, the heavier, fatter babies from diabetic pregnancies were also hyperinsulinemic [7]. Pathophysiology of GDMThe exact mechanisms behind GDM still remain unclear. The following maternal and fetal-placental factors are interrelated and act in an integrated manner in the development of insulin resistance and GDM. The Role of the Fetal-Placental Unit in the Development of GDMDuring pregnancy, as gestational age progresses, the size of the placenta increases. There is a rise in the levels of pregnancy-associated hormones like estrogen, progesterone, cortisol and placental lactogen in the maternal circulation [8,9] accompanied by an increasing insulin resistance. This usually begins between 20 and 24 weeks of gestation. As the mother goes through parturition and delivers the fetus, the placental hormone production stops, and so does the illness of GDM, which strongly suggests that these hormones cause GDM [10]. Human placental lactogen raises approximately 10-fold in the second half of the pregnancy. It stimulates lipolysis, which leads to an increase in free fatty acids in order to provide a different fuel to the mother and to conserve glucose and amino acids for the fetus. In turn, the increase in free fatty acid levels directly interferes with the insulin-directed entry of glucose into cells. Therefore, human placental lactogen is considered as a potent antagonist of insulin action during pregnancy. The Role of Adipose Tissue in the Development of GDMAdipose tissue produces adipocytokines, including leptin, adiponectin, tumor necrosis factor-α (TNF-α) and interleukin-6, as well as the newly discovered resistin, visfatin and apelin [11,12]. The roles of adipocytokines and elevated lipid concentrations in pregnancy have also been associated with the changes in insulin sensitivity in nonpregnant women [13] as well as in pregnant women [14]. Evidence suggests that one or more of these adipokines might impair insulin signaling and cause insulin resistance [12]. Specifically, TNF-α has a potential role in decreasing insulin sensitivity [15]. Modified Pedersen's HypothesisThe pathophysiology of macrosomia can be explained based on Pedersen's hypothesis of maternal hyperglycemia leading to fetal hyperinsulinemia and increased utilization of glucose and, hence, increased fetal adipose tissue. When maternal glycemic control is impaired and the maternal serum glucose level is high, the glucose crosses the placenta. However, the maternal-derived or exogenously administered insulin does not cross the placenta. As a result, in the second trimester, the fetal pancreas, which is now capable of secreting insulin, starts to respond to hyperglycemia and secrete insulin in an autonomous fashion regardless of glucose stimulation. This combination of hyperinsulinemia (insulin being a major anabolic hormone) and hyperglycemia (glucose being a major anabolic fuel) leads to an increase in the fat and protein stores of the fetus, resulting in macrosomia (fig. 1). Fig. 1Results of maternal hyperglycemia modified according to Pedersen's hypothesis. Macrosomia-Related ComplicationsMaternal ComplicationsIf the baby is atypically large, vaginal birth will be more complicated. There is a risk of prolonged labor in which the fetus might be stuck in the birth canal, instrumental delivery (with forceps or vacuum) may be needed, and even unplanned or emergency cesarean section may be necessary. During birth, there is a greater risk of laceration and tear of the vaginal tissue than when the baby is of normal size, and the muscle between the vagina and the anus might tear (perineal tear). There is also a high chance of uterine atony. The uterus muscle may not properly contract, resulting in heavy bleeding and postpartum hemorrhage. The risk of postpartum bleeding and genital tract injury was about 3-5 times higher in macrosomic deliveries [16]. Besides, if the mother has had a previous cesarean section, there is a higher chance of uterus tear along the scar line of the previous surgery. Fetal ComplicationsImmediate Complications Premature Birth. Due to early induction of labor before 39 weeks of gestation and/or premature rupture of membranes, there is a risk of preterm delivery. Although all the necessary precautions are undertaken prior to induction of early labor, newborns are still under the risk of complications associated with prematurity, including difficulties in respiration and feeding, infection, jaundice, neonatal intensive care unit admission and perinatal death. Shoulder Dystocia and Erb's Palsy. One of the most serious complications of vaginal delivery in macrosomic babies is shoulder dystocia which is associated with birth trauma. Newborns with a birth weight of 4,500 g or more carry a 6 times higher risk of birth trauma [17], and the risk of brachial plexus injury is approximately 20 times higher when the birth weight is above 4,500 g [18]. Hypoglycemia at Birth. One of the most common metabolic disorders of the neonate of a GDM mother is hypoglycemia. It occurs due to the hyperinsulinemia of the fetus in response to the maternal hyperglycemia in utero. Hypoglycemia can lead to more serious complications like severe central nervous system and cardiopulmonary disturbances. Major long-term sequelae include neurologic damage resulting in mental retardation, recurrent seizure activity, developmental delay and personality disorders. Neonatal Jaundice. Factors which may account for jaundice are prematurity, impaired hepatic conjugation of bilirubin and increased enterohepatic circulation of bilirubin resulting from poor feeding. In macrosomia, neonates have a high oxygen demand causing increased erythropoiesis and, ultimately, polycythemia. Therefore, when these cells break down, bilirubin (a byproduct of red blood cells) increases resulting in neonatal jaundice. Congenital Anomalies. Heart defects and neural tube defects, such as spina bifida, are the most common types of birth defects. The high blood sugar level of women with GDM can damage the developing organs of the fetus, leading to congenital anomalies. Later Complications Childhood Obesity and Metabolic Syndrome. Many studies suggest that one of the reasons of childhood obesity is GDM. There has been evidence of fetal programming of later adiposity amongst offspring exposed to existing diabetes in utero. The offspring of Pima Indian women with preexisting type II diabetes and GDM were larger for gestational age at birth and, after approximately 5 years of age, were heavier than the offspring of prediabetic or nondiabetic women [19]. The Exploring Perinatal Outcomes among Children (EPOCH) study found that exposure to maternal GDM was associated with a higher BMI, a greater waist circumference, more visceral and subcutaneous adipose tissue and a more centralized fat distribution pattern in 6- to 13-year-old multiethnic youth [20]. Moreover, youth exposed to maternal GDM in utero had an overall higher average BMI growth from 27 months through 13 years of age and a higher BMI growth velocity starting at age 10-13 years [21]. These findings suggest that the long-term effects of in utero GDM exposure are not always evident in early childhood, but rather emerge during puberty, another sensitive period for the development of obesity. Offspring of diabetic mothers is also susceptible to the onset of metabolic syndromes such as increased blood pressure, hyperglycemia, obesity and abnormal cholesterol levels that occur together and increase the risk of heart disease, stroke and diabetes. Transgenerational Transmission of GDM and EpigeneticsIn GDM, the abnormal metabolic intrauterine environment affects the development of the fetus by inducing changes in gene expression by epigenetic mechanisms of susceptible cells, leading to the development of diabetes in adulthood. Offspring (F1 generation) of severely and mildly hyperglycemic mothers develops GDM and other metabolic disorders in later life, affecting the second generation (F2 generation) as well. Thus, GDM gives rise to a vicious cycle in which mothers with GDM have babies with epigenetic changes who are prone to develop metabolic disease later in life, which will give rise to a new generation of mothers with GDM. This trend of passing a disease from one generation to another through epigenetic changes is known as transgenerational transmission (fig. 2). Fig. 2Vicious cycle of transgenerational transmission of GDM. It is now widely accepted that an adverse preconceptional and intrauterine environment is associated with epigenetic malprogramming of the fetal metabolism and predisposition to chronic, and in particular, metabolic disorders later in life [22,23]. Epigenetics is the study of heritable changes in gene expression that occur without changes in the DNA sequence [24]. DNA methylation and histone modifications are two major epigenetic regulators in mammalian cells, which are functionally linked in transcription and may provide a mechanism for the stable propagation of gene activity from one generation of cells to the next [25]. Biochemical changes, i.e. in the form of DNA methylation and histone modifications, control the spatial, temporal and parent-specific highly coordinated gene expression patterns. As exogenous influences can induce epigenetic modifications, epigenetic variation among individuals may be genetically or environmentally determined [26]. Many different studies have made the observation that early adverse conditions are associated with diabetes and metabolic dysfunction later in life. Although the mechanisms involved in the epigenetic modifications that lead to the possibility of transgenerational transmission are still unclear, evidence suggests that methylation in germ cells might be responsible [27]. Others suggested that the hyperglycemic uterine environment during pregnancy affects multiple loci in the fetal epigenome initiating metabolic programming, leading not only to transgenerational transmission of GDM but also of several other metabolic diseases [28,29]. In one study [30], in both F1 and F2 offspring of GDM mothers in a rat model, the expression of imprinted genes Igf2 and H19 was downregulated in pancreatic islets, which was caused by the abnormal methylation status of the differentially methylated region, which may be one of the mechanisms for impaired islet ultrastructure and function. Furthermore, in the same study, altered Igf2 and H19 gene expression was found in sperm of adult F1 GDM offspring, indicating that changes of epigenetics in germ cells contributed to transgenerational transmission. In another study [28], to test the effects of GDM on the epigenome of the next generation, cord blood and the placenta of mothers with GDM were tested. Here, the maternally imprinted MEST gene, the nonimprinted glucocorticoid receptor NR3C1 gene and interspersed ALU repeats showed significantly decreased methylation levels in GDM groups compared to controls. Significantly decreased blood MEST methylation was also observed in adults with morbid obesity compared to normal-weight controls, suggesting that epigenetic malprogramming of MEST may contribute to obesity predisposition throughout life. Several studies on different genes were carried out in order to understand the epigenetic mechanisms of GDM and transgenerational transformation. All of these studies found epigenetic alterations in the respective genes which had been studied [28,31,32,33,34]. Therefore, from these studies, we can conclude that epigenetic mechanisms predispose offspring to developing type II diabetes, GDM and other metabolic diseases in later stages of life. An increased need for insulin by the fetus to deal with high levels of glucose caused by GDM is an environmental circumstance which probably triggers epigenetic changes in the early stage of life, involving genes critical to pancreatic development and B-cell function, peripheral glucose uptake and insulin resistance. Maternal Obesity, GDM and MacrosomiaThe majority of mothers with GDM are obese, and a significant proportion of those who are obese have GDM [35]. One meta-analysis showed that the risk of developing GDM was 2.14-fold higher in overweight pregnant women, 3.56-fold higher in obese pregnant women and 8.56-fold higher in severely obese pregnant women compared to pregnant women with normal weight [36]. An analysis of data from more than 23,000 women in the HAPO (Hyperglycemia and Adverse Pregnancy Outcomes) study [37] showed that the prevalence of macrosomia among 17,244 nonobese women without GDM was 6.7% compared to 10.2% in 2,791 nonobese women with GDM and 20.2% in 935 obese women with GDM. A study has shown that maternal obesity is a stronger predictor of a large-for-gestational-age infant than maternal hyperglycemia [38]. In the HAPO study [37], the investigators found that the frequency of macrosomia in GDM was increased by 50% compared to non-GDM in both the nonobese and obese groups. Obesity was associated with a 2-fold higher frequency of macrosomia whether in the non-GDM or GDM group. Macrosomia in GDM only was present in 26%, in GDM plus obesity in 33% and in obesity only in 41%. A large prospective study from Spain found that the upper quartile of maternal BMI was responsible for 23% of macrosomia, while GDM accounted for 3.8% [39]. Women who did not have GDM but who were obese had a 13.6% increased risk of macrosomia (defined as a child weighing 4,000 g or more at birth) than nonobese women [37]. From this, we can conclude that although GDM and maternal obesity are independently associated with adverse pregnancy outcomes, the combination of both GDM and maternal obesity has a greater effect on macrosomia. Management of MacrosomiaThere are various recommendations for the management of macrosomia varying from expectant management and elective induction of labor before term to elective cesarean section for an estimated fetal weight of ≥4,250 g [40] or >4,500 g [41] depending on the study. Studies have shown that the chance of vaginal delivery is higher when spontaneous labor occurs than when labor is inducted [42]. However, waiting for spontaneous labor to begin is an option limited by gestational age. As the gestational age exceeds 41 weeks of gestation, maternal morbidity and perinatal morbidity and mortality increase. Hence, timely action to induct delivery is needed. Early Induction of LaborGiven that after 37 weeks of gestation the fetus continues to grow at a rate of 230 g/week [43], elective induction of labor before or near term has been proposed to prevent macrosomia and its complications [44]. However, there are two factors necessary for the induction of labor: the first is fetal lung maturation. Fetuses with a diabetic mother have been shown to have delayed lung maturity. Normally, the pulmonary maturation takes place at a mean gestational age of 34-35 weeks. By 37 weeks, 99% of fetuses are matured. However, in the fetus of a diabetic mother, the lung may not be mature until 38.5 weeks. The second important point is that the patient who is going to undergo induction must have a ripe cervix with a Bishop score of ≥6; otherwise, there is an increased chance of failure of induction, which ultimately leads to a cesarean section [45]. In one study [46], the outcomes of suspected macrosomic infants of mothers who had expectant management of pregnancy versus elective induction of labor were compared. The rate of cesarean sections was found to be very high (57 vs. 31%) in those who were assigned to the electively inducted group. In some studies, elective induction of labor for macrosomia was found to increase the rate of cesarean delivery without improvement in perinatal outcomes [42,47]. Elective Cesarean SectionMany studies suggest offering a cesarean section to patients who are suspected of expecting a macrosomic infant, especially to those with GDM, insulin-dependent diabetes and a previous high-birth-weight infant, so as to prevent maternal and fetal birth trauma. Unfortunately, measures to calculate the weight of the fetus are inaccurate [48]. In one study, it was claimed that, in a general population, it is unreasonable to perform an elective cesarean section to prevent brachial plexopathy [49]. Management of the NeonateLarge-for-gestational-age neonates do not only include postterm infants, but also term or even preterm infants. This should be kept in mind as the management and the main concerns in treatment could differ. A strictly regulated maternal blood sugar level decreases the perinatal adverse outcomes. Neonates with a diabetic mother should undergo a full physical examination from head to toe, congenital anomalies (congenital heart defects, tracheoesophageal fistula and central nervous system abnormalities) and birth trauma being of more concern. They should receive intensive observation and care and should be evaluated for hypoglycemia, polycythemia, hyperbilirubinemia and electrolyte abnormalities. The blood glucose level should be examined within 1 h of life, then every hour for the next 6-8 h and then as needed. Oral feeding, ideally breast feeding, is recommended as soon as possible, and if oral feeding is insufficient, an intravenous infusion of glucose should be started. Disclosure StatementNone of the authors has any conflicts of interest in connection with this study. Copyright: All rights reserved. No part of this publication may be translated into other languages, reproduced or utilized in any form or by any means, electronic or mechanical,
including photocopying, recording, microcopying, or by any information storage and retrieval system, without permission in writing from the publisher. What do we monitor when a baby is born to a diabetic mother?Your healthcare provider will screen you for gestational diabetes between 24 and 28 weeks of pregnancy. This screening is done using an oral glucose tolerance test (OGTT). An OGTT checks a woman's blood sugar levels after she has sugar (glucose).
What is the most common abnormality found in the infant of a diabetic mother?The most common defects occurred in the cardiovascular system, NTDs, cleft lip/palate and skeletal defects. Although many studies discuss diabetes associated congenital anomalies, the leading type of birth defects and the exact rate of diabetes associated birth defects are difficult to determine.
|