Gestational diabetes (pronounced jess-TAY-shun-ul die-uh-BEET-eez) is one of the most common health problems for pregnant women. It affects about 5 percent of all pregnancies, which means there are about 200,000 cases each year. If not treated, gestational diabetes can cause health problems for mother and fetus. Show
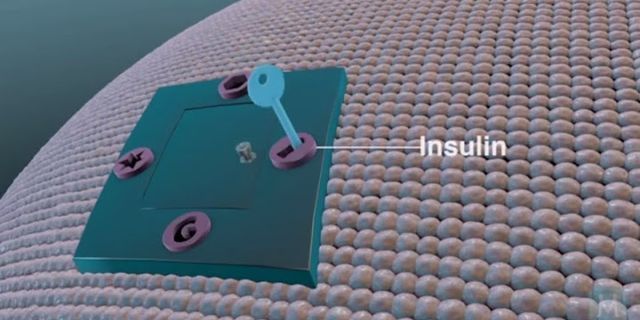
The good news is that gestational diabetes can be treated, especially if it is found early in the pregnancy. There are some things that women with gestational diabetes can do to keep themselves well and their pregnancies healthy. Controlling gestational diabetes is the key to a healthy pregnancy. and can be achieved by following the Gestational Diabetes Treatment Plan. Gestational Diabetes is a kind of diabetes that only pregnant women get. In fact, the word gestational means “during pregnancy.” If a woman gets diabetes or high blood sugar when she is pregnant, it is gestational diabetes. DiabetesDiabetes means your blood sugar is too high. Diabetes is a disease of metabolism, which is the way your body uses food for energy and growth. Your stomach and intestines break down (or digest) much of the food you eat into a simple sugar called glucose (pronounced GLOO-kos). Glucose is your body’s main source of energy. After digestion, the glucose passes into your bloodstream, which is why glucose is also called blood sugar. Once in the blood, the glucose is ready for your body cells to use. However, your cells need insulin (pronounced IN-suh-lin), a hormone made by your body, to get the glucose. Insulin “opens” your cells so that glucose can get in. When your metabolism is normal, your body makes enough insulin to move all the glucose smoothly from your bloodstream into your cells. If you have diabetes, your body does not make enough insulin and your cells can’t use insulin properly. This causes the glucose to builds up in your bloodstream. The Difference Between Diabetes and Gestational DiabetesOnly pregnant women get gestational diabetes. When you are pregnant, your body goes through many changes that can make it difficult for your insulin to work properly. Your body cannot get the sugar out of your blood and into your cells to use for energy as well as it did before. The placenta, a system of vessels that passes nutrients, blood, and water from mother to fetus, makes certain hormones that prevent insulin from working correctly. This is insulin resistance. Your body has to make three times its normal amount of insulin or more to overcome the hormones made by the placenta. For most women, the body’s extra insulin is enough to keep their blood sugar levels in the healthy range. For about 5 percent of pregnant women, even the extra insulin is not enough to keep their blood sugar level normal. Testing for gestational diabetes is done between the 24th and 28th week of pregnancy. Will gestational diabetes hurt my baby?If not treated, gestational diabetes can lead to health problems. The best way to promote a healthy pregnancy if you have gestational diabetes is to follow the treatment plan outlined by your health care provider. Most women who have gestational diabetes give birth to healthy babies, especially when they keep their blood sugar under control, eat a healthy diet, get regular, moderate physical activity, and gain the right amount of weight. In some cases, though, the condition can affect the pregnancy. Keeping glucose levels under control may prevent certain problems related to gestational diabetes. Below are some conditions that can result from your having gestational diabetes. Keep in mind that just because you have gestational diabetes does not mean that these problems will occur. Macrosomia (pronounced mak-row-SOHM-ee-uh)—Baby’s body is larger than normal. Large-bodied babies can have difficulty by natural delivery through the vagina; the baby may need to be delivered through cesarean section. The most common complication for these babies is shoulder dystocia (pronounced dis-TOE-shee-uh). Hypoglycemia (pronounced high-po-gl-eye-SEEM-ee-uh)—Baby’s blood sugar is too low. You may need to start breastfeeding right away to get more glucose into the baby’s system. If it is not possible for you to start feedings, the baby may need to get glucose through a thin, plastic tube in his or her arm that puts glucose directly into the blood. Jaundice (pronounced JAWN-diss)—Baby’s skin turns yellowish; white parts of the eyes may also change color slightly. If treated, jaundice is not a serious problem for the baby. Respiratory Distress Syndrome (RDS)—Baby has trouble breathing. The baby might need oxygen or other help breathing if he or she has RDS. Low Calcium and Magnesium Levels in the Baby’s Blood—Baby could develop a condition that causes spasms in the hands and feet, or twitching or cramping muscles. This condition can be treated with calcium and magnesium supplements. Will gestational diabetes affect my labor and delivery?Most women with gestational diabetes can make it to their due dates safely and begin labor naturally. In some cases, though, gestational diabetes could change the way you feel or how your baby is delivered. Having gestational diabetes does not mean that you will have any change in delivery. If you have gestational diabetes, there are things you should know about delivery:
Will I have diabetes after I have my baby?Once you have the baby, your body should be able to use its insulin more effectively. Shortly after the baby is born, the placenta is “delivered.” (This is sometimes called the afterbirth.) Because the placenta causes insulin resistance, when it’s gone, gestational diabetes usually goes away, too. If you have gestational diabetes, you are at higher-than-normal risk for developing type 2 diabetes later in your life. Type 2 diabetes, like gestational diabetes, occurs when the body doesn’t use its insulin properly. Eating a healthy diet, keeping your weight within a healthy range and getting regular physical activity after your baby is born can help lower your risk for type 2 diabetes. Who can I go to for help with gestational diabetes?Women who have gestational diabetes benefit most from a team approach, which may include management and treatment of the condition. Your team may include obstetricians, advanced practice nurses, registered nurses, a registered dietitian and certified diabetes educator. How does diabetes during pregnancy affect a fetus?Diabetes that is not well controlled causes the baby's blood sugar to be high. The baby is “overfed” and grows extra large. Besides causing discomfort to the woman during the last few months of pregnancy, an extra large baby can lead to problems during delivery for both the mother and the baby.
What are fetal complications from maternal diabetes that the nurse must monitor for?Fetal complications include preterm labor and delivery, small or large size for gestational age, shoulder dystocia birth injury, and neonatal hypoglycemia.
What are the 3 main concerns with unmanaged gestational diabetes for the fetus?Blood sugar that is not well controlled in a woman with gestational diabetes can lead to problems for the pregnant woman and the baby:. An Extra-Large Baby. ... . C-Section (Cesarean Section) ... . High Blood Pressure (Preeclampsia) ... . Low Blood Sugar (Hypoglycemia) ... . 5 Tips for Women with Gestational Diabetes. ... . More Information.. Which are risk factors of diabetes in pregnancy?The known risk factors for Gestational Diabetes Mellitus (GDM) are advanced age (≥35 yrs.), overweight or obesity, excessive gestational weight gain, excessive central body fat deposition, family history of diabetes, short stature (<1.50 m), excessive fetal growth, polyhydramnios, hypertension or preeclampsia in the ...
|